Guest post written by: Vivek Mandan
The Key to Ending the Autoimmune Epidemic
Most of us know firsthand that despite the estimated 50 million Americans with at least one or more autoimmune diseases, public awareness is practically nonexistent. How could this be? 50 million individuals out of a national population of 320 million is almost 16%. With almost one-sixth of the nation suffering, autoimmune disease is undeniably an epidemic – yet, medical treatment remains limited and research scarce and disorganized. How did this happen silently and unnoticed when we have the most advanced medical knowledge in the history of the world? Let’s dissect this snapshot of the medical status of modern autoimmunity by answering two critical questions: how did we get here and how do we move forward?
Autoimmunity and Medical Specialization
The medical system is segmented into specialties. If someone has a hormonal issue, they go to an endocrinologist; kidneys, a nephrologist; digestion, a gastroenterologist. There are immense benefits to specialization – with a system as complex as the human body, it is impossible to make any progress without systematic specialization.
However, autoimmune diseases were only recognized as a class of disease around 60 years ago in 1957, long after the creation of medical specialties. Since autoimmune diseases tend to affect multiple biological systems and have a shared etiology, dividing autoimmune diseases by the primary physiological location in which the worst symptoms manifest is both inefficient and inaccurate with regards to treatment and research.
This mismatch between specialized providers and multifaceted diseases becomes clearer as we examine the numbers surrounding research and treatment. Currently, autoimmune disease related healthcare expenses come to over $100 billion per year, while cancer costs come to $57 billion. However, research funding for autoimmune diseases are a paltry $850 million, compared to the $5.4 billion for cancer. Why is the funding for cancer over 6 times that of autoimmune diseases, while the healthcare expense of autoimmune diseases is nearly double that of cancer?
Cancers have been grouped together as a class of disease when it comes to research and treatment. While individual treatments vary, investigating the common factors between various cancers has led to tremendous progress in understanding the mechanisms behind them. It’s time to do the same for autoimmune diseases. Autoimmune disease research is fragmented – Hashimoto’s is researched as a thyroid disease, psoriasis as a skin disorder, rheumatoid arthritis as a joint disease. In order to understand autoimmune diseases, the first step is to group them together. For more information, check out Dr. Bonnie Feldman’s excellent article.
Lab tests and the patient experience
The other major challenge in autoimmune disease research is the lack of comprehensive patient information. People with autoimmune diseases tend to have many symptoms that aren’t alleviated by standard medical treatment. As a result, many individuals start doing research on their own to see if diet, lifestyle changes, supplements, and more can make a positive impact on their quality of life. If you have an autoimmune disease, and you’re reading this, you probably fall into this category.
The disconnect occurs because researchers and healthcare providers are unable to effectively access a scientific, well organized form of individual information. There is currently no lab test or combination of tests that can account for the myriad symptoms and treatments that patients experience throughout their time outside of the doctor’s office. The problem is somewhat cyclical – research is stifled by inefficient organization of disease information and patients can’t centralize their information without new research technology that addresses the entirety of their condition. How can we make progress and move past this standstill?
Like a Pedometer for the 21st Century
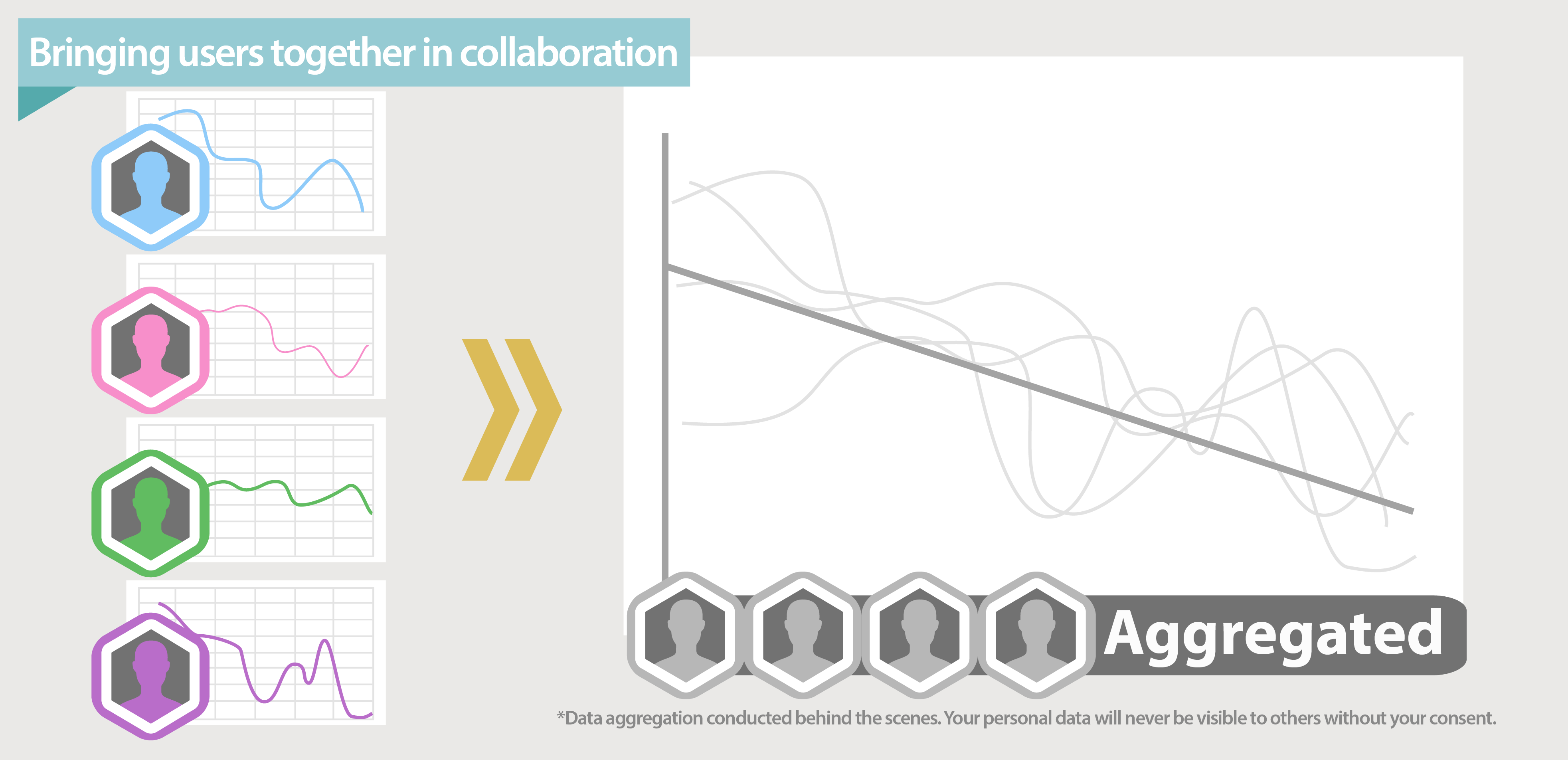
New relationships between autoimmune diseases cannot be gleaned without first establishing a crystal clear picture of each patient’s specific situation. Mobile/web software can make this a reality. Over 68% of American adults have a smartphone, enabling us as a community to gather an unprecedented amount of information, which is why Autoimmune Citizen Science is developing a tool capable of individualized health tracking and powerful data aggregation for autoimmune diseases. As individuals track their daily progress, we can employ data aggregation – the gathering of information for the purpose of statistical analysis – to compare patient experiences across the community as a whole, thus revealing patterns and correlations.
With the AICS app, you’ll be able to track everything you’re trying (medications, diet, supplements, and more) and study how it affects your symptoms and lab tests in detail. The app is first and foremost a tool to help you make sense of your health. While you focus on tracking your daily progress, we’ll be aggregating the data across everyone who uses the app (anonymously and privately) giving you immediate access to real statistics based on real data. This way you’ll be able to see what’s working for other people with the same symptoms and conditions. What we love about this app is that it helps citizen scientists manage their autoimmune diseases right away, and at the same time uses the data they provide to make progress for the entire autoimmune community.
Citizen science is the key to ending the autoimmune epidemic. Through seeing what people with autoimmune diseases are going through and trying on a daily basis, we take the first step toward understanding how to solve the mystery behind these illnesses. The AICS app is currently under development and we have our first beta release planned for May 22nd. If you’re interested in learning more, check out our interview with Petra Chambers-Sinclair. Want to be a beta user? Sign up here. We hope to see you join us as a citizen scientist today.
-Vivek




My autoimmune symptoms vary considerably based on mind-body connection. When I am in touch with my body’s needs I am significantly better. I’d like to explore this as a key part of the ‘treatments’ for AI conditions