Guest post and images written and created by: Mitch Beito
Wrongly Accused
Lactate, or its protonated counterpart, lactic acid, has long been touted as the scapegoat for the soreness experienced after training. However, delayed-onset muscle soreness (DOMS), or what most people call “second-day sore,” is actually part of the inflammatory response induced to repair the muscle micro-tears inflicted during exercise. Lactate does increase in concentration as muscle fatigue begins to set in, but recent research suggests this to only be a mere proxy of fatigue rather than a causative agent. In fact, it seems as though lactate is found in the bloodstream in some amount at all times (not just during exercise), indicating that it is being produced around the clock and may be much more than a waste product of anaerobic respiration.
Skeletal Muscle Energetics and Physiology
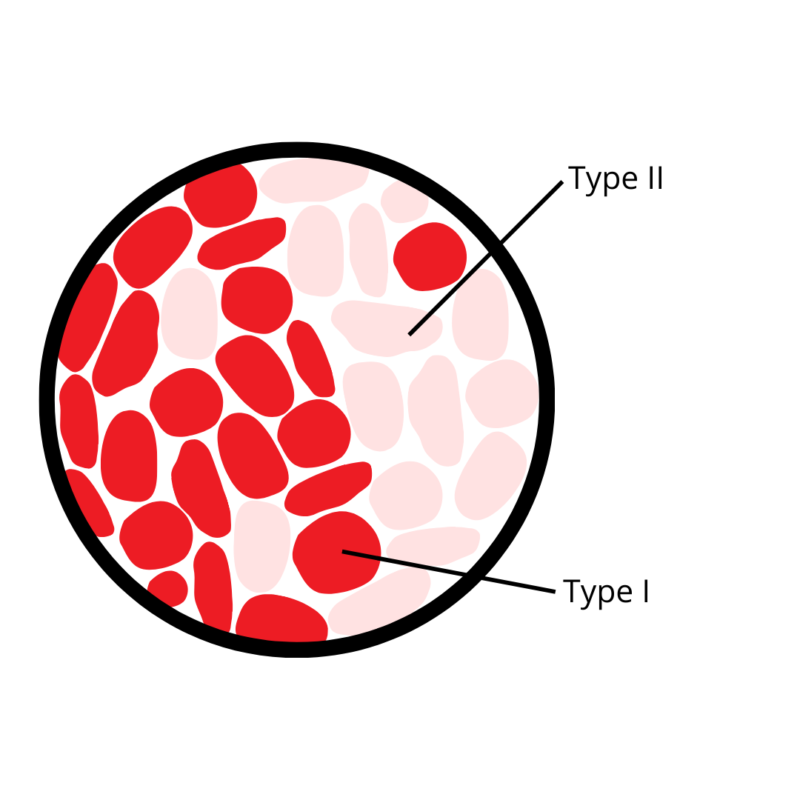
Every muscle is composed of some ratio of slow-twitch (Type I) to fast-twitch (Type II) fibers. The difference between the two is not that they twitch or contract at different speeds, but that they twitch with a different force. The fast and slow designation simply refers to how fast the two fatigue. That being said, slow-twitch fibers are associated with endurance, while fast-twitch fibers allow for explosive movements such those found in sprinting or weight lifting.
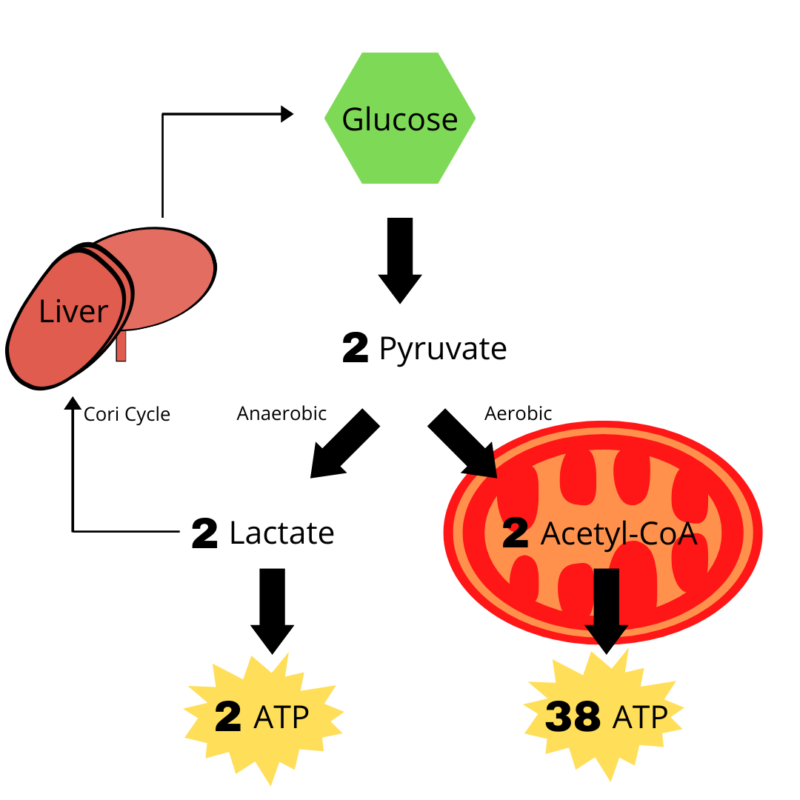
 These fibers also differ in their metabolism. Slow-twitch respire predominantly through aerobic respiration (consuming oxygen) and fast-twitch through anaerobic respiration (not consuming oxygen). At the end of glucose metabolism (a process known as glycolysis) two molecules of pyruvate are produced. Under aerobic conditions, this pyruvate enters the mitochondria where it undergoes oxidative phosphorylation to yield 38 ATP of cellular energy. On the other hand, if oxygen is not readily available, pyruvate is converted to lactate allowing for a much quicker, albeit less efficient way of metabolizing glucose, netting only 2 ATP per cycle.
These fibers also differ in their metabolism. Slow-twitch respire predominantly through aerobic respiration (consuming oxygen) and fast-twitch through anaerobic respiration (not consuming oxygen). At the end of glucose metabolism (a process known as glycolysis) two molecules of pyruvate are produced. Under aerobic conditions, this pyruvate enters the mitochondria where it undergoes oxidative phosphorylation to yield 38 ATP of cellular energy. On the other hand, if oxygen is not readily available, pyruvate is converted to lactate allowing for a much quicker, albeit less efficient way of metabolizing glucose, netting only 2 ATP per cycle.
Under normal conditions, respiration occurs aerobically, but if one were to suddenly bust out a pull-up or sprint down the drive-way, the oxygen that one breathes in would likely not be available to the muscle and hence this energy would be supplied by anaerobic means. Because of its inefficiency however, these types of movements cannot be sustained for long periods of time. This switch makes sense from an evolutionary standpoint to avoid sustaining irreparable damage to muscle tissue, but has long perplexed scientists as to why cancer cells seem to make this same switch.
Warburg Effect and Utilization of Lactate
The Warburg Effect describes this seemingly contradictory preference that cancer cells have for the inefficiency associated with anaerobic glycolysis. The name is based on Otto Warburg’s observations in 1923 of cancer cell metabolism, illustrating that lactate production was independent of the presence of oxygen. Warburg hypothesized that mitochondrial dysfunction could be the reasoning behind this transition, and hence provide some insight into the likelihood of carcinogenic development based on one’s mitochondrial health. However, recent work by Dr. Iñigo San-Millán and Dr. George A. Brooks (doi:10.1093/carcin/bgw127) has suggested that lactate production through anaerobic means provides an ideal environment for cancer cells to flourish.
All excess lactate was previously thought to be converted back into glucose through the Cori cycle where it could then be stored in the liver, and finally released into the bloodstream at a moment’s notice. Now, lactate is acknowledged as a potent signalling molecule that could influence gene expression through tightly regulated feedback networks.
Increased lactate levels are the byproduct of both inactivation of pyruvate dehydrogenase (enzyme that normally converts pyruvate to acetyl-CoA rather than lactate under aerobic conditions) and overexpression of lactate dehydrogenase (enzyme that converts pyruvate to lactate under anaerobic conditions). Once produced, lactate is anything but stationary. It has been shown to upregulate the expression of monocarboxylate transporters (specifically MCT4) which effectively efflux lactate from tumor cells. This may lead to several downstream effects such as:
- Increasing angiogenesis and tumor blood supply through stimulating vascular endothelial growth factor (VEGF)
- Promoting cancer cell migration and metastasis by inducing the expression of transforming growth factor-β2 (TGF-β2)
- Cancer cells evading the immune system by decreasing cytokine production of T-cells
- Providing a constant supply of glucose to cancer cells by increasing glutaminolysis, or the conversion of the amino acid glutamine to glucose when glycogen reserves are depleted
- Allowing tumor-promoting oncogenes to be transported to other cells of the body by creating an acidic extracellular environment for exosome release
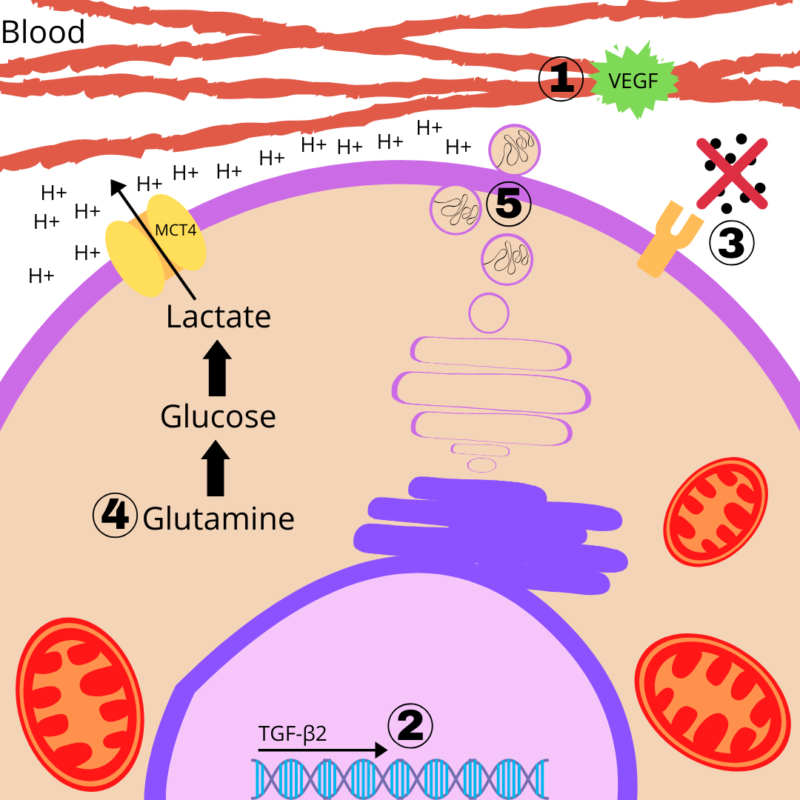
Each of these five effects have presented themselves in malignant tumors and are characteristic changes that occur during cancer development at the cellular level. The review paper mentioned above has found each of these effects to be associated with increased lactate levels. With this knowledge, new anticancer drugs are being developed to target and inhibit MCTs, barring these downstream effects from occurring. But as many have already expressed, if there was a pill that elicited the same effects as exercise, everyone would be taking it.
Effects of Exercise on Lactate
It seems as though with increased exercise, the goal may not be so much as producing less lactate while working out, but rather conferring ways to clear lactate from the blood as quickly as possible or limiting the amount that enters the blood in the first place. While the efflux of lactate into the bloodstream can be converted back to glucose through the Cori cycle, this process takes time to complete. It would be much more efficient to recycle this lactate at the level of the muscle, ensuring a quicker turnover of lactate and preventing its accumulation in the blood. In fact, elite athletes have been shown to have some of the lowest lactate levels in their bloodstream at any given time.
MCT4 is upregulated in Type II fast-twitch fibers, allowing for this efflux of lactate to occur. However, Type I slow-twitch fibers are now known to be the primary driver of lactate clearance, ensuring lactate does not build up in the blood. Another monocarboxylate transporter, MCT1, is found to be upregulated in these slow-twitch fibers. As opposed to MCT4, MCT1 allows lactate to enter these fibers. Once inside, it may diffuse into the mitochondria and be converted to pyruvate by an enzyme called mitochondrial lactate dehydrogenase (mLDH).
How can this process be improved and ensure that lactate is following this route? Endurance training has shown to increase the number of MCT1, the expression of mLDH, and mitochondrial biogenesis. Thus, the lactate that is produced is quickly cleared and may easily be converted to a fuel source without ever leaving the muscle. Lactate testing may provide the most information regarding how well individuals may perform in training and competition. Low lactate levels both during physical activity and at rest could be indicative of not only better performance, but also the level of risk one may have for developing cancer. Exercise has shown to limit lactate accumulation by improving the efficiency of muscle energetics, and by doing so, may play a monumental role in cancer prevention.
Guest post written and images created by: Mitch Beito

Join the Discussion