Guest post written by: Carolyn Dolan
This is a topic near and dear to my heart. I have been hesitant to share this condition because it honestly scared me to death when I first learned about it. In time, not only have I healed, but the more I understand the condition the more empowered I become to prevent it from coming back.
This is a lengthy research report, so bare with me as the details are important. I will describe the condition leaky gut (or increased intestinal permeability), how it is linked to your immune system, why it matters, causes and solutions.
Leaky gut is more specifically described as increased intestinal permeability. It is a descriptive term related to the small intestines having a reduced barrier function. This condition is not a diagnosis alone, but has been linked to many illness and symptomology.
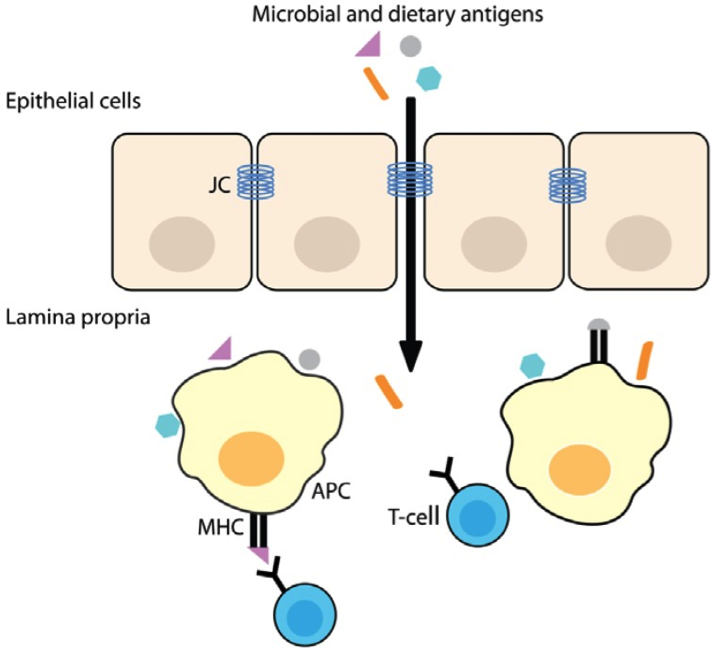
The small intestines allows properly digested fats, proteins and starches to pass through the cells in order to be used by the body while providing a barrier to keep out foreign substances, large undigested molecules and bacterial products. Gastrointestinal mucosal lining and microscopic villi (little hair like tentacles) provides the barrier function of the small intestines. In between the epithelial cells are tight junctions held together by the junctional complex. When the junctional complex is disrupted, the epithelial cells separate and allow particles into the body without policing them. Once the particles enter the body, the immune system recognizes those particles as foreign (an antigen) and stimulates an antibody reaction.1
This patency of the small intestines provides a direct access to our cellular immune system. The antigens (either dietary related or microbial or viral) pass through the weakened junctional complex(JC), they are presented by an antigen-presenting cell (APC) to the T-cells (a lymphocyte produced by the Thymus gland). 1
This is your direct access to the cell-mediated immune response as well as inflammatory response. Below is a figure of the process of the antigens getting through the leaky gut wall and the immune response.
How do you test for this condition?
To officially test for intestinal permeability, the standard is to perform a lactulose/mannitol test. One would ingest the permeability marker orally (lactulose/mannitol) and then measure the contents in the urine. 2 Other permeability markers have been tested in a mice model including FITC-dextran 400 and ovalbumin measured in the plasma as well as polyethylene glycol measured in the urine. All oral permeability tests have been shown to be suitable in assessing intestinal barrier function. 3
Once intestinal permeability is increased and a leaky gut is present, the antigen enters the body and stimulates the cell-mediated immune response. It is important to understand, at this point, the symptoms related to this response could be anywhere and dramatically vary from individual to individual and day to day. Another indicator of increased intestinal permeability/leaky gut is any one or more of the associated symptoms or clues4:
Abdominal pain
Anxiety
Asthma
Bed wetting
Chronic joint pain
Chronic muscle pain
Confusion
Constipation
Diarrhea
Fatigue
Fevers
Fuzzy thinking
Gas
Indigestion
Poor immunity
Poor memory
Recurrent Bladder Infections
Shortness of Breath
Toxic feelings
This intestinal permeability condition has been linked to many diagnoses as a potential contributor to the disease process. It stands to reason that there may be a cause and effect relationship, but that continues to be the debate. Here are a few diagnosis that have been linked to increased gut permeability:
Depression5
Obesity5
Diabetes Type 25
Intestinal Inflammation (Crohn’s, Ulcerative Colitis, Celiac Disease)6
Juvenile Chronic Arthritis7
Parkinson’s Disease8
Non-alcoholic Fatty Liver Disease9
Rheumatoid Arthritis10
Relapsing-Remitting Multiple Sclerosis11
Ankylosing Spondylitis12
Eosinophilic Oesophagitis 13
Bronchial Asthma 14
Food Allergy15
Schizophrenia16
Aortic Dissection17
Many more conditions have been associated with a leaky gut. To be honest, I began to run out of time to validate each condition. The reality is that research continues to elucidate this topic.
What I am particularly interested in is to understand what CAUSES the small intestines to become “leaky” and setting up the immune response, which may correlate with disease. I will address four categories related to cause based on the soar principles of Eat Well, Move Well, Sleep Well, and Soar On.
Food Causes
It should be of no surprise to anyone reading this, if you follow my blog, that the first food component I will address is wheat and gluten containing grains as a cause of increased intestinal permeability. Gliadin is a gluten protein contained in wheat and other grains like rye and barley that have been targeted in celiac disease(read more here http://www.renosoar.com/holistic-health-tips/to-eat-gluten-or-not-to-eat-gluten-that-is-the-question).
A recent published study took biopsy specimens from small intestines of adult subjects undergoing an esophagogastroduodonscopy (EGD) for various reasons. Each subject was categorized as either a celiac patient with active disease (ACD), celiac patient in remission (RCD), non-celiac patient with gluten sensitivity (GS), and non-celiac control (NC). Each biopsy was incubated with gliadin or media alone. The researchers found that all biopsies demonstrated increased intestinal permeability in all groups in the presence of gliadin. However, the greatest increase occurred in the samples from the ACD group, which was no different from the GS group. 18
“Increased intestinal permeability after gliadin exposure occurs in all individuals.” 18
The proposed mechanism is related to the disruption of the junctional complex described above via the zonulin pathway as a direct result of the presence of gluten proteins, not just the presence of intestinal inflammation. 19 What I find of particular interest regarding the gluten grains is that despite their link to increased intestinal permeability and a variety of symptoms that those grains remain difficult to give up for many without a specific celiac diagnosis. It has been proposed that gluten grains may even “mask” their own toxicity by having an opioid effect. The gluten can be degraded into morphine-like substances called gluten exorphins. These compounds could cover up the deleterious effects of gluten on the gastrointestinal lining. 20
Basically, gluten-containing grains may act like addictive drugs.
Unfortunately, the food causes of increased intestinal permeability do not stop with gluten-grains. In a mouse study evaluating the growth of intestinal tumors compared high fat diet (defined as 45% of fat calories) to a normal diet (defined as 15% of fat calories) composed of corn oil and lard. The high fat diet had increased oxidative stress as well as an increased membrane permeability of the intestinal lining via the zonulin pathway. 21 I have spoken to healthy fat in the past. Corn oil is considered an unstaturated fatty acid that can become trans when heated as it is unstable. As compared to lard which is more heat stable and in moderation and sourced optimally can be health promoting. These points may be potentially important in the case of intestinal integrity because not all fats are created equally. See more here on (http://www.renosoar.com/holistic-health-tips/fat-is-it-really-health-promoting)
Another food like substance that is associated with increased intestinal permeability is food additives. Processed foods are high in food additives to optimize texture, color, sweetness, taste and shelf stability. Specifically, glucose, salt, emulsifiers, organic solvents, gluten (again;)), microbial transglutaminase and nanoparticles (very small) have been tied to increased intestinal permeability by breaching the junctional complex. 22 This is particularly problematic for children that consume prepackaged snacks for convenience sake morning, noon and night. This unfortunate habit common for parents puts them at an even higher risk for incidence of autoimmune diseases and any of the above-mentioned diseases.
Exercise Causes
Most would consider exercise in nearly all ways, beneficial. Yet, I found an interesting correlation with increased intestinal permeability in heavy exercise and exertional heatstroke. In a study of 8 healthy male subjects that were regular exercisers were subjected to 20 min of constant speed on a treadmill equivalent to 80% of VO2 max as determined per each subject. Within 5 min of the run, they were subjected to an oral intestinal permeability test. This workout was associated with increased permeability. 23 Later we will discus their protocol to decrease the intestinal permeability.
Heatstroke is considered catastrophic as a result of heat-related illness and is most common in a younger person engaging in strenuous activity in a warm environment. The stress of the exercise in a hot environment will reduce the blood flow to the intestines and promote a reduction in the junctional complex resulting in increased permeability and other local and systemic inflammatory reactions that result in endotoxemia. 24-26 This condition is rare, but the consequences may be deadly. This extreme exercise condition however, is a cause of increased intestinal permeability.
Another component that I am putting in this category as it relates to movement outside in the sun. Vitamin D is produced naturally with the UVB rays hitting the skin and converting cholesterol into Vitamin D. In today’s world, Vitamin D deficiency is more and more prevalent. Vitamin D is not only important in modulating the immune system, but it also protects the mucosal barrier of the intestines. In a mouse study comparing Vitamin D rich diet or deficient diet, they found that Vitamin D provided a strengthening of the intestinal epithelial wall against infections that are known to increase permeability like E. Coli. 27,28 Although it is not a direct causal effect on intestinal permeability it appears that Vitamin D deficiency reduces the resistance to developing leaky gut in the presence of an infection like C-Diff.
Sleep Causes
As I have described in the past, our sleep patterns are regulated by our circadian rhythm. Disruption of the circadian clock has been associated to many disorders, now to include a disruption of the intestinal epithelial barrier. A mouse study used an alcohol induced leaky gut model and found that disruption of the sleep-wake cycle promoted further gut leakiness in the mouse. 29
Interestingly, in a human study evaluating intestinal permeability in night shift workers with day shift workers that alcohol consumption did not alone induce intestinal permeability. However, they found that the night shift workers had elevated inflammatory markers and an increased risk for developing intestinal permeability in the presence of alcohol. The sleep architecture played a role in developing a higher risk for increased intestinal permeability in the presence of social drinking. 30 There is speculation that the circadian genes control the expression of several genes involved in regulating intestinal permeability and that can be induced by alcohol. 31
Soaring Causes
The fourth principle is Soar On, which is where purpose and connection live. In this category is also where I will put psychological stress. I have spoken to stress before here (http://www.renosoar.com/holistic-health-tips/5-reasons-stress-is-good-for-you) mostly as it is related to improving all aspects of your life. However, unchecked stress can build up and become problematic especially in the presence of painkillers. A mouse study evaluated the effect of psychological stress exacerbating nonsteroidal anti-inflammatory drug (NSAID) induced small bowel injury. The psychological stress, as a result of water avoidance, increased intestinal permeability in the presence of NSAID enteropathy as well as changing the microbiota. 32 It would appear that psychological stress unchecked might increase intestinal permeability.
Now that we can understand that the development of increased intestinal permeability or leaky gut has a variety of causes and risk factors, the question is, what can we do to resolve the problem or decrease intestinal permeability? It turns out that the solution is in the cause.
Eat Well – Solution
The first step in relation to healing leaky gut, is to remove the potential triggers like gluten, refined food products containing additives, and trans fats. Eating organic whole fruits and vegetables alongside healthy protein sources will be critical in the recovery of the intestinal integrity.
There are some other supplements that may facilitate permeability resistance, enhancing tight junctions, improving the microbiome and healing:
Zinc Carnosine with Bovine Colostrum23
Whey protein33
L-Glutamine34,35
Saturated Fat36
Omega 3 fatty acids36
Bifidobacterium bifidum37
Some whole food options that contain many of these beneficial supplement components are wild oily fish (omega 3), fermented foods like sauerkraut (probiotic), organic raw whole dairy (whey), pastured lard/ghee/butter (saturated fat), and bone broth (glutamine).
Remove. Replace. Restore.
Remove gluten grains, trans fats and refined food products.
Replace with whole nutrient rich fruits, vegetables and proteins. Include organic raw dairy if tolerated, wild caught oily fish like sardines, fermented foods like sauerkraut to re-inocculate the gut, bone broth and pasture-raised fats.
Restore tight junction integrity.
Move Well – Solution
Exercise has a multitude of benefits like strengthen muscle, improve mood, improve bone strength, improve wound healing, burn fat, and potentially slow aging. The World Health Organization recommends 150 minutes of moderate aerobic activity weekly and muscle strengthening twice a week. This could include playing with your kids, gardening or walking the dog. High intensity is considered short burst of all out exercise is as effective as longer workouts.
If you find yourself in the high-intensity exercise over long duration group putting you at risk, then the specific movement recommendation to restore gut integrity would be rest. The decrease in vagal activity helps to lower the risk of chronic disease and decrease the intestinal epithelial permeability.38
A rat study looked at the influence on the tight junctions in the ileum following endurance exercise. For the rat, the exercise was a treadmill for 60 min/day for 10 days at a work rate of 70% maximum oxygen consumption. This amount of exercise improved antioxidant enzymes and tight junction proteins as well as reduce inflammatory markers. 39 Although this doesn’t directly correlate with humans, one could safely assume that regular moderate-exercise (not extended high intensity in the heat) would likely produce similar results.
As I described above and describe in the book Soar Into Health, the importance of Vitamin D cannot be ignored. As stated previously, Vitamin D is a natural conversion of blood cholesterol in the presence of UVB spectrum sunlight hitting the skin. Specifically related to intestinal permeability, Vitamin D3 has been shown to preserve epithelial barrier function in the presence of intestinal injury, be it Crohn’s disease or ethanol-induced. 40-43 The free source of vitamin D3 is full sun exposure to a majority of your skin, without burning. Yet, during certain times of the year or even job requirements, it is not possible to get the needed skin exposure to produce adequate and therapeutic amounts. You can check your area at
www.aa.usno.navy.mil/data/docs.AltAz.php for when the sun is above the 50 deg altitude in order to provide UV B exposure for Vitamin D conversion.
If you are unable to get the needed exposure, then supplementation is a safe and maybe necessary option. A randomized double-blind placebo-controlled study in patients with Crohn’s disease found that 2000IU supplementation of D3 significantly increased blood levels and decreased intestinal permeability. 43
There is debate on what plasma level of Vitamin D3 is optimal and safe. A recent literature review report, evaluted the target values and upper limits of Vitmain D. The authors concluded the dose recommendation be based on body weight. They did conclude that serum 25(OH)D concentrations higher than 210 nmol/L as undesirable, but that 50 nmol/L is safe. 44
Below are two charts from www.vitamindcouncil.org that may help guide you personally as I would recommend testing your levels before supplementing and then retest after a period of time of supplementation. Remember that Vitamin D is a fat-soluble vitamin so a carrier fat is required when supplementing and D3 is the form most absorbable.
Vitamin D 25(OH)D range guidelines from various organizations:
| Vitamin D Council | Endocrine Society | Food and Nutrition Board | Testing Laboratories | |
| Deficient | 0-30 ng/ml | 0-20 ng/ml | 0-11 ng/ml | 0-31 ng/ml |
| Insufficient | 31-39 ng/ml | 21-29 ng/ml | 12-20 ng/ml | |
| Sufficient | 40-80 ng/ml | 30-100 ng/ml | >20 ng/ml | 32-100 ng/ml |
| Toxic | >150 ng/ml |
The Vitamin D Council suggests that a level of 50 ng/ml is the ideal level to aim for. This is why the Council recommends that adults take 5,000 IU/day of vitamin D supplement in order to reach and stay at this level.
Recommended daily intakes from various organizations:
| Vitamin D Council | Endocrine Society | Food and Nutrition Board | |
| Infants | 1,000 IU/day | 400-1,000 IU/day | 400 IU/day |
| Children | 1,000 IU/day per 25lbs of body weight | 600-1,000 IU/day | 600 IU/day |
| Adults | 5,000 IU/day | 1,500-2,000 IU/day | 600 IU/day, 800 IU/day for seniors |
The Food and Nutrition Board recommended daily intakes are the official recommendations by the United States government.
Can eating foods high in Vitamin D help raise my plasma levels?
Yes, eating foods high in Vitamin D like mushrooms and sardines is helpful. It is difficult, if not impossible, to reach the above recommendations on food alone especially in the absence of UV B sun rays.
Remove. Replace. Restore.
Remove avoidance of the sun and excessive intense exercise.
Replace with adequate skin exposure and supplement if needed to reach therapeutic Vitamin D3 levels. Exercise moderately, and sometimes intensely for short bursts with sufficient REST in between. Everyday life movement counts as exercise and has health benefits.
Restore intestinal integrity and resistance to infections.
Sleep well – Solution
As I described in Soar Into Health, sleep is critical for rest and recovery. Although sleep is characterized by a reduction in consciousness it is not the absence of activity. As I searched specifically for the benefits of sleep on the intestinal integrity, I came up empty handed for that specific condition. However, I did find a report that validated the idea that sleep has a direct effect on peripheral tissues, which includes, but not limited to, heart, lung, and likely gastrointestinal tissue as well. Sleep actually enhances organ specific molecular functions by reducing metabolic stress. Sleep may even synchronize all of our organs.45
The amount of sleep required for each individual varies based on age and lifestyle. As a general rule, waking on your own feeling rested in the morning is an indication of adequate sleep. The amount for adults 26-64 years is 7-9 hours. 46 Given the habit of sleep deprivation in our culture, I recommend determining the hour you need to wake and count back 9 hours for determining bedtime. More details can be found in Soar Into Health. A few tips to optimize sleep are:
Keep your bedroom cool (60-72 F).
Keep your room dark, dark, dark.
Turn off all screens 1-2 hours before determined bedtime.
Keep all screens out of the bedroom.
Get natural sunshine in the morning and during the day.
Make bedtime a routine.
Eat Well.
Move well.
Remove. Replace. Restore.
Remove sleep disruptors and regular late nights
Replace with a regular bedtime in a dark room to allow for a minimum of 8-9 hours of sleep so you wake rested.
Restore a synchronous healing process…including your intestinal lining.
Soar On –Solutions
As I described earlier that physiological stress may increase intestinal permeability. You may ask yourself, how is it possible to address the stressful life components when they are out of your control? For example, being a parent requires managing many young children who are dependent on you and short of leaving, there is no way to change that responsibility or stress. The same goes for many professionals. Stress is a part of life. Although your perception of stress plays a role in how your body handles stress, how can you improve your intestinal permeability by reducing stress that is often a fixed part of life?
Much like sleep, I was unable to find a direct resource demonstrating a decreased in intestinal permeability with stress reduction techniques. What I did find is a study using mindfulness-based program for resilience training in healthcare professionals. The pilot-program included eight weeks on mindfulness program combining meditation with nutrition and exercise resulting in a reduction in stress, depression and anxiety47 (all symptoms that could be correlated with leaky gut syndrome.)
Another study evaluated women healing from breast cancer, a clearly stressful diagnosis, found that 20-sessions of contemplative self-healing improved quality of life and decreased symptoms of post-traumatic stress.48
Although these particular studies were not directly related to intestinal permeability, they do indicate the powerfulness of meditative or self-healing as a means for relieving symptoms of stress.
As a clinician, I often recommended a simple 10 min practice of diaphragmatic breathing as a potential for calming the nervous system and triggering the body to reduce vagus nerve stimulation, which is often associated with increased pain states. Performing simple activities to calm the nervous system have only benefits to release stress without removing your life stress…like kids.
A study from an alternative journal reported a decrease in blood viscosity (a potential risk factor for cardiovascular disease) with earthing (grounding) by simply exposing the human body to the surface of the earth. Although this experiment used an artificial grounding model of electrical stimulation, 49 I like the idea of simply putting your bare feet on the earth, or even hugging a tree. Better yet, go walk in the sunshine through the trees to get grounded and release the pent up stress.
Stress is what makes our lives more beautiful. Yet, ignoring the impact of stress in your life and attempting to ignore it, exercise it away, or eating junk food may be counter productive when it comes to leaky gut. The best way to release stress is a personal proposition. Some things that may help release stress are:
Prayer
Meditation
Talking with a good friend or family member
Diaphragmatic Breathing
Walking in nature
Touching the earth
Hugging a pet or loved one
Crying
Singing
In the end, it’s personal. Finding your release only takes trial and error.
Remove. Replace. Restore.
Remove anxiety about stress in your life
Replace with a means to release the stress in your life. Try different ideas to find one that fits your personality and lifestyle, but commit to it regularly if not daily.
Restore a healthy gut…even with stress in your life.
Eat Well. Move Well. Sleep Well. Soar On….to heal a leaky gut.
References:
- de Punder K, Pruimboom L. The dietary intake of wheat and other cereal grains and their role in inflammation. Nutrients. 2013;5(3):771-787.
- Kohlstadt I, ed. Advancing medicine with food and nutrients. Second ed. Voca Raton, FL: Taylor and Francis Group, LLC; 2013.
- Volynets V, Reichold A, Bardos G, Rings A, Bleich A, Bischoff SC. Assessment of the intestinal barrier with five different permeability tests in healthy C57BL/6J and BALB/cJ mice. Dig Dis Sci. 2016;61(3):737-746.
- Lipski, Elizabeth PhD CCn CHN. Digestive wellness. 4th Edition ed. United States of America: Mc GRaw Hill; 2012.
- Slyepchenko A, Maes M, Machado-Veira R, et al. Intestinal dysbiosis, gut hyperpermeability and bacterial translocation: Missing links between depression, obesity and type 2 diabetes? Curr Pharm Des. 2016.
- Luettig J, Rosenthal R, Barmeyer C, Schulzke JD. Claudin-2 as a mediator of leaky gut barrier during intestinal inflammation. Tissue Barriers. 2015;3(1-2):e977176.
- Picco P, Gattorno M, Marchese N, et al. Increased gut permeability in juvenile chronic arthritides. A multivariate analysis of the diagnostic parameters. Clin Exp Rheumatol. 2000;18(6):773-778.
- Clairembault T, Leclair-Visonneau L, Coron E, et al. Structural alterations of the intestinal epithelial barrier in parkinson’s disease. Acta Neuropathol Commun. 2015;3:12-015-0196-0.
- Mao JW, Tang HY, Zhao T, et al. Intestinal mucosal barrier dysfunction participates in the progress of nonalcoholic fatty liver disease. Int J Clin Exp Pathol. 2015;8(4):3648-3658.
- Lerner A, Matthias T. Rheumatoid arthritis-celiac disease relationship: Joints get that gut feeling. Autoimmun Rev. 2015;14(11):1038-1047.
- Buscarinu MC, Cerasoli B, Annibali V, et al. Altered intestinal permeability in patients with relapsing-remitting multiple sclerosis: A pilot study. Mult Scler. 2016.
- Vaile JH, Meddings JB, Yacyshyn BR, Russell AS, Maksymowych WP. Bowel permeability and CD45RO expression on circulating CD20+ B cells in patients with ankylosing spondylitis and their relatives. J Rheumatol. 1999;26(1):128-135.
- Katzka DA, Geno DM, Blair HE, Lamsam JL, Alexander JA, Camilleri M. Small intestinal permeability in patients with eosinophilic oesophagitis during active phase and remission. Gut. 2015;64(4):538-543.
- Hijazi Z, Molla AM, Al-Habashi H, Muawad WM, Molla AM, Sharma PN. Intestinal permeability is increased in bronchial asthma. Arch Dis Child. 2004;89(3):227-229.
- Chen T, Liu X, Ma L, et al. Food allergens affect the intestinal tight junction permeability in inducing intestinal food allergy in rats. Asian Pac J Allergy Immunol. 2014;32(4):345-353.
- Lambert MT, Bjarnason I, Connelly J, et al. Small intestine permeability in schizophrenia. Br J Psychiatry. 1989;155:619-622.
- Gu J, Hu J, Qian H, et al. Intestinal barrier dysfunction: A novel therapeutic target for inflammatory response in acute stanford type A aortic dissection. J Cardiovasc Pharmacol Ther. 2016;21(1):64-69.
- Hollon J, Puppa EL, Greenwald B, Goldberg E, Guerrerio A, Fasano A. Effect of gliadin on permeability of intestinal biopsy explants from celiac disease patients and patients with non-celiac gluten sensitivity. Nutrients. 2015;7(3):1565-1576.
- de Punder K, Pruimboom L. The dietary intake of wheat and other cereal grains and their role in inflammation. Nutrients. 2013;5(3):771-787.
- Pruimboom L, de Punder K. The opioid effects of gluten exorphins: Asymptomatic celiac disease. J Health Popul Nutr. 2015;33:24-015-0032-y.
- Park MY, Kim MY, Seo YR, Kim JS, Sung MK. High-fat diet accelerates intestinal tumorigenesis through disrupting intestinal cell membrane integrity. J Cancer Prev. 2016;21(2):95-103.
- Lerner A, Matthias T. Changes in intestinal tight junction permeability associated with industrial food additives explain the rising incidence of autoimmune disease. Autoimmun Rev. 2015;14(6):479-489.
- Davison G, Marchbank T, March DS, Thatcher R, Playford RJ. Zinc carnosine works with bovine colostrum in truncating heavy exercise-induced increase in gut permeability in healthy volunteers. Am J Clin Nutr. 2016;104(2):526-536.
- Lambert GP. Stress-induced gastrointestinal barrier dysfunction and its inflammatory effects. J Anim Sci. 2009;87(14 Suppl):E101-8.
- Lambert GP. Intestinal barrier dysfunction, endotoxemia, and gastrointestinal symptoms: The ‘canary in the coal mine’ during exercise-heat stress? Med Sport Sci. 2008;53:61-73.
- Lambert GP. Role of gastrointestinal permeability in exertional heatstroke. Exerc Sport Sci Rev. 2004;32(4):185-190.
- Assa A, Vong L, Pinnell LJ, Avitzur N, Johnson-Henry KC, Sherman PM. Vitamin D deficiency promotes epithelial barrier dysfunction and intestinal inflammation. J Infect Dis. 2014;210(8):1296-1305.
- Assa A, Vong L, Pinnell LJ, et al. Vitamin D deficiency predisposes to adherent-invasive escherichia coli-induced barrier dysfunction and experimental colonic injury. Inflamm Bowel Dis. 2015;21(2):297-306.
- Summa KC, Voigt RM, Forsyth CB, et al. Disruption of the circadian clock in mice increases intestinal permeability and promotes alcohol-induced hepatic pathology and inflammation. PLoS One. 2013;8(6):e67102.
- Swanson GR, Gorenz A, Shaikh M, et al. Night workers with circadian misalignment are susceptible to alcohol-induced intestinal hyperpermeability with social drinking. Am J Physiol Gastrointest Liver Physiol. 2016;311(1):G192-201.
- Swanson G, Forsyth CB, Tang Y, et al. Role of intestinal circadian genes in alcohol-induced gut leakiness. Alcohol Clin Exp Res. 2011;35(7):1305-1314.
- Yoshikawa K, Kurihara C, Furuhashi H, et al. Psychological stress exacerbates NSAID-induced small bowel injury by inducing changes in intestinal microbiota and permeability via glucocorticoid receptor signaling. J Gastroenterol. 2016.
- Xiao K, Jiao L, Cao S, Song Z, Hu C, Han X. Whey protein concentrate enhances intestinal integrity and influences transforming growth factor-beta1 and mitogen-activated protein kinase signalling pathways in piglets after lipopolysaccharide challenge. Br J Nutr. 2016;115(6):984-993.
- Wang B, Wu Z, Ji Y, Sun K, Dai Z, Wu G. L-glutamine enhances tight junction integrity by activating CaMK kinase 2-AMP-activated protein kinase signaling in intestinal porcine epithelial cells. J Nutr. 2016;146(3):501-508.
- Wang H, Zhang C, Wu G, et al. Glutamine enhances tight junction protein expression and modulates corticotropin-releasing factor signaling in the jejunum of weanling piglets. J Nutr. 2015;145(1):25-31.
- Lam YY, Ha CW, Hoffmann JM, et al. Effects of dietary fat profile on gut permeability and microbiota and their relationships with metabolic changes in mice. Obesity (Silver Spring). 2015;23(7):1429-1439.
- Hsieh CY, Osaka T, Moriyama E, Date Y, Kikuchi J, Tsuneda S. Strengthening of the intestinal epithelial tight junction by bifidobacterium bifidum. Physiol Rep. 2015;3(3):10.14814/phy2.12327.
- Van Houten JM, Wessells RJ, Lujan HL, DiCarlo SE. My gut feeling says rest: Increased intestinal permeability contributes to chronic diseases in high-intensity exercisers. Med Hypotheses. 2015;85(6):882-886.
- Holland AM, Hyatt HW, Smuder AJ, et al. Influence of endurance exercise training on antioxidant enzymes, tight junction proteins, and inflammatory markers in the rat ileum. BMC Res Notes. 2015;8:514-015-1500-6.
- Chen S, Zhu J, Chen G, et al. 1,25-dihydroxyvitamin D3 preserves intestinal epithelial barrier function from TNF-alpha induced injury via suppression of NF-kB p65 mediated MLCK-P-MLC signaling pathway. Biochem Biophys Res Commun. 2015;460(3):873-878.
- Du J, Chen Y, Shi Y, et al. 1,25-dihydroxyvitamin D protects intestinal epithelial barrier by regulating the myosin light chain kinase signaling pathway. Inflamm Bowel Dis. 2015;21(11):2495-2506.
- Chen SW, Ma YY, Zhu J, et al. Protective effect of 1,25-dihydroxyvitamin D3 on ethanol-induced intestinal barrier injury both in vitro and in vivo. Toxicol Lett. 2015;237(2):79-88.
- Raftery T, Martineau AR, Greiller CL, et al. Effects of vitamin D supplementation on intestinal permeability, cathelicidin and disease markers in crohn’s disease: Results from a randomised double-blind placebo-controlled study. United European Gastroenterol J. 2015;3(3):294-302.
- Veugelers PJ, Pham TM, Ekwaru JP. Optimal vitamin D supplementation doses that minimize the risk for both low and high serum 25-hydroxyvitamin D concentrations in the general population. Nutrients. 2015;7(12):10189-10208.
- Anafi RC, Pellegrino R, Shockley KR, Romer M, Tufik S, Pack AI. Sleep is not just for the brain: Transcriptional responses to sleep in peripheral tissues. BMC Genomics. 2013;14:362-2164-14-362.
- National Sleep Foundation. sleepfoundation.org.
- Johnson JR, Emmons HC, Rivard RL, Griffin KH, Dusek JA. Resilience training: A pilot study of a mindfulness-based program with depressed healthcare professionals. Explore (NY). 2015;11(6):433-444.
- Charlson ME, Loizzo J, Moadel A, et al. Contemplative self healing in women breast cancer survivors: A pilot study in underserved minority women shows improvement in quality of life and reduced stress. BMC Complement Altern Med. 2014;14:349-6882-14-349.
- Chevalier G, Sinatra ST, Oschman JL, Delany RM. Earthing (grounding) the human body reduces blood viscosity-a major factor in cardiovascular disease. J Altern Complement Med. 2013;19(2):102-110.

Great informative post! I would add the importance of vitamin K2 here, especially if you’re supplementing with vitamin D (also, there’s some new research coming out that lower vitamin D levels are actually OK, and D can be dangerous above 50, with 20-50 as the ideal range. See Chris Kresser’s most recent vitamin D post).
Great post! Re. Vit. D, I did an experiment to help me determine my optimal Vit D level. I had my D level tested at the end of last winter (69.3 ng/mL). I stopped supplementing (4,500 IUs daily), and started laying in the sun, nude, for 20 mins a day when the sun was above 50 degrees altitude. After 3 months, I took another D test (53.1 ng/m).. Since the body cannot “over produce” D to a toxic level by sun alone, I figure if the low-50’s is where my body is with sun exposure only (and the little I get from sardines or pastured lard), maybe it is best I supplement only to that level, and not above, during the fall/winter months. I have reduced my supplementing to 3,000 IUs daily. Will test again at the end of this winter.. Sounds logical, anyone out there know if this “experiment” I did is valid? That it gives me a ballpark target level for optimal D, both in my body and for supplementation?
Thank You for sharing this very informative, practical, action-oriented and documented article. Outstanding!
I have Celiac Disease and I need to lose weight. Need help with my diet
This is really good information, especially about vitamin D and stress. I think stress is often overlooked when it comes to gut problems