Well, hysteria from Old Theresa and Eddie not withstanding, it looks like the mechanism for leaky gut and the autoimmune response gets clearer by the day. Pedro sent me this paper which describes the association pretty clearly. It has a few gems which we will get to in a moment. The study involved the analysis of 33 people with Type 1 diabetes, all of whom had normal intestinal architecture. I emphasize this point because theoretically, a biopsy is the “gold standard” test for Celiac, which appears to be the only clinically acknowledged form of gluten intolerance. The more common method of diagnosis is a blood anti-body test which is less than worthless IMO. Here are a few interesting lines from the paper:
Mounting evidence suggests that the gut immune system is involved in the development of autoimmune diabetes. An inflammatory state has been demonstrated to be present in the structurally normal intestine of patients with type 1 diabetes, and the abnormal intestinal permeability that has been found in these patients could represent a contributing factor.
What this means is these people had an active autoimmune disease but appeared to be negative on the conventional diagnostic tests such as biopsy and serum antibody. Most doctors and those who dismiss a role for grains in autoimmunity would have stopped here. But when we dig a little deeper we find some interesting things:
Immunofluorescence studies showed that 11 of 14 type 1 diabetic children with elevated levels and 11 of 19 with normal serum levels of anti-TG2 antibodies presented with mucosal deposits of such autoantibodies. The phage display analysis technique confirmed the intestinal production of the anti-TG2 antibodies
So almost every single kid with serum positive anti-gluten antibodies showed a positive response in the gut tissues (not too surprising even for those who think gluten only affects 1 in 125 people, but keep in mind, all of these kids were STILL negative on the gold standard of intestinal villi damage) but the really surprising thing was the kids who had no serum antibodies showed significant response in gut tissue. Here is all that stated again, plus some more fun:
These subjects with signs of a deranged immune response to gliadin may be considered potential celiac disease patients; in fact, some of the type 1 diabetic patients who are negative for celiac disease–associated autoantibodies may later become seropositive and may eventually develop frank enteropathy.
It has recently been shown that specific celiac disease autoantibodies against TG2 are deposited in the normal jejunal mucosa before they can be detected in the circulation and that their deposition precedes the gluten-induced jejunal lesion. This finding raises the possibility that the anti-TG2 antibodies might be located only at the small mucosal level in some type 1 diabetic patients.
I know it’s kinda thick, technical stuff but what this paper indicates is when a doctor (or anyone else) sits back and dismisses the gut autoimmune connection for Type 1 diabetes (or any other autoimmune disease) they are really missing the boat. At one time it was assumed celiac only affected 1 in 15,000. then it was 1 in 1,500 now the official story is something like 1 in 125. This is all bullocks, this issue affects everyone, it just manifests differently in different people. One of the main antibodies they talk about in the paper, TG2, (trans glutaminase) is an enzyme that alters EVERY PROTEIN IN THE BODY. This is why one pathological vector (leaky gut) can manifest in so many different ways (all the autoimmune diseases known and unknown).
The gold standard in all this should be: remove grains, legumes and dairy and see if the individual improves, lab work be damned.
Interestingly, weighing and measuring gluten containing foods does not mitigate it’s effects…so much for Nutritional Astrology.
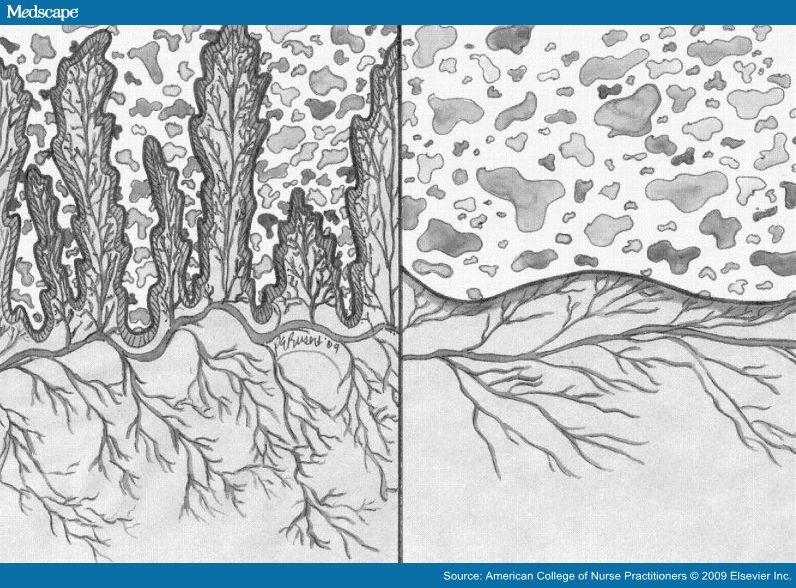
Normal vs. Abnormal (celiac) intestinal mucosa

Robb!!!!!!
This post is killer! I have been digging through some similar stuff lately
http://www.informaworld.com/smpp/content~db=all~content=a713996127
http://www.ncbi.nlm.nih.gov/pubmed/19758171
But the paper from Pedro is on the ball. I am sending this post to a Type 1 I know as we speak. Thanks alot man! Keep this thing rollin!
Last but not least…love the bit on the zone…
Ben-
thanks brother! Let your friend know there are several type 1 posts in the archive.
Ahh…the Zone…
An interesting tidbit from the paper:
“All of the type 1 diabetic patients were observed to be HLA-DQ2 and/or -DQ8 positive”
Robb, any opinion on stool antibody testing for gluten sensitivity? The paper appears to be in line with the concept.
Stephen-
Yes, but again you need a fairly advanced condition already in place to shed enough antibodies to get a positive test. One could be quite ill but still sub-clinical. I’m all for a variety of lab diagnostics but I’m still of a mind to simply recommend elimination to see if a myriad of symptoms improves.
Great post Robb!
I think it is so unfortunate when medical types give people the advice to keep eating gluten until there is damage to the villi, so that a “proper diagnosis” is made of what is pretty much an end-stage manifestation of a gluten problem…letting a person suffer unnecessarily for years. This is asinine, like saying to an overweight person, “keep eating a dozen donuts a day until you are morbidly obese. Then at that point you should change your diet, but not until then, so we know for sure you’re fat.” Sounds stupid but I think it is the same.
Sarah-
Yep, I suspect 5-10 years from now this position will really change in the medical community, but that’s a long time to wait.
Robb,
I definitely agree that improvements after eliminating gluten are the ultimate indication of gluten sensitivity, regardless of test results.
WOW that is a great research article! I hope the scientists find out more about dietary antigens, the gut immune system, and type 1 diabetes. It’s not just cereal grains though, I’m pretty sure dairy is another important factor.
The gluten/gliadin-T1D connection is an interesting one, and I haven’t heard that much about it until very recently. The theory that I’m more familiar with involves beta casein A1 as a factor. There have been several epidemiological studies that have linked cow’s milk to T1D (although epi studies on diet tend to be flawed and hard to interpret.)
I would like to see some time course studies- understanding the progression of the disease from preclinical to overt T1D with respect to pancreatic and intestinal damage might give us a better idea of which one comes first. My bet is on pro-inflammatory wheat and casein peptides as a contributing factor in disease progression.
For now, though, it’s hard to say for sure that either casein or gluten is truly causative. It is also possible that T1D is a general autoimmune disorder in which the intestinal epithelium is an innocent bystander and a victim of hyperglycemia- its destruction leads to leaky gut and then you get introduction of antigens into the lamina propria, which triggers antibody production.
Sorry ‘bout the long comment, I get all excited when I see science posts…
NikkiT
This is an awesome article. Im a type 1 vegan diabetic and I just recently removed gluten from my diet about 1 1/2 months ago. I feel so much better its amazing. My insulin requirements are lower and my sugars don’t swing up and down.
Why are legumes bad to eat? Do they do the same thing as gluten?
Tony-
Yep, they have similar problems. Tty adding 5,000iu of vit d3 daily and see how that influences things.
After 4 straight days of my daughter( who was diagnosed with type 1 diabetes at age 5, 4 years ago) having normal to low blood sugar on 7 and a half units of insulin total for a 24 hour period- we went out to eat for mother’s day. She and I had salads and a cup of chili and I did the carb counting thing and gave her extra insulin and pow- she shot up to 500, and today she keeps going up to 300. I’m sure it was either the beans in the chili or something in the salad dressing. Last night and this morning, she has eaten only a good diet- nuts seeds, green smoothies, small bit of chicken and veggies fried in coconut oil. I hope I haven’t messed her up with one meal and that her insulin requirements don’t start creeping up again.
Another high blood sugar trigger was a multivitamin that had soy, milk, fructose, sorbitol, and xylitol. When she used to take them she’d shoot up to 300 almost immediately after. I didn’t suspect them because they only have 1 gram of carbs. Now I’m almost sure they spiked her blood sugar because she took one on a day off from school and told me she thinks the vitamin spiked her blood sugar and sure enough she was 300 again! She was 89 before the vitamin. I know her food could have affected her blood sugar but she had her usual veggies and an egg fried in coconut oil which has never raised her blood sugar above normal levels.
JanieG-
It could be a food allergy, not necessarily a vitamin. But it could also be a B vit. The lectins in beans are nasty, nasty.
She bounced back a few days after Mother’s day. She almost always has decent numbers now on about 9 units of insulin. We switched her vitamins and she doesn’t spike high after them now, and we avoid beans. If she drinks water with fresh squeezed lemon in it she doesn’t need insulin for her trail mix- which is 100% raw nuts( no peanuts). She can also eat trail mix without insulin if she eats a salad with it. But give her the trail mix on its own and you have to give her insulin with it.
We continue to work toward someday reducing her insulin but she and I are happy so far with seeing better numbers and keeping her dosage at 10 units or less. I’ll keep you posted if she ever takes a turn for the better.
Hey Robb, great article. When you say, “remove grains, legumes and dairy and see if the individual improves” how long is long enough to see results? I am recommending to a friend with Type 1 Diabetes that she gives paleo a shot, but I know the first question is going to be “how long before I see something.”
Thanks
Brian
4-6 weeks. Get sleep dialed (dark room etc) would also recommend making sure vit-d levels are within the 60-80ng/dl range. All in the book.
This is an interesting post. I have been type 1 for 18 yrs. I was diagnosed with Celiac at age 5. The symptoms of Celiac “went away” by age 10. I developed Type 1 by age 17. Interesting…eh.
I have a degree in Food Science and Human Nutrition. The education system is training RD’s with the wrong info. The Food Guide Pyramid should be illegal. Then again its main purpose is to slowly get the masses sick –> prescribe medicine and continue the process. There is no money in Healthy people.
I have been moving toward a diet of raw and organic for over a year. My insulin intake has been reduced by 2/3’s. I have had to ignore the educational foundation that was given to me at university.
how are you doing with your diet? i am diabetic slowly going paleo and paleo type workouts at the gym and noticing better insulin sensitivity and i have reduced my insulin requirements by 50%